PDF of lecture notes~

Dysautonomia Symptoms & Treatment
Dysautonomia is a complex and often misunderstood condition that affects the Autonomic Nervous System (ANS), which controls essential bodily functions without conscious thought. As a healthcare professional with experience in treating hundreds of dysautonomia cases, I have encountered countless patients who have gone from doctor to doctor, often being misdiagnosed with anxiety or depression. It’s frustrating for them, but with the right approach, there is hope.
Understanding Dysautonomia
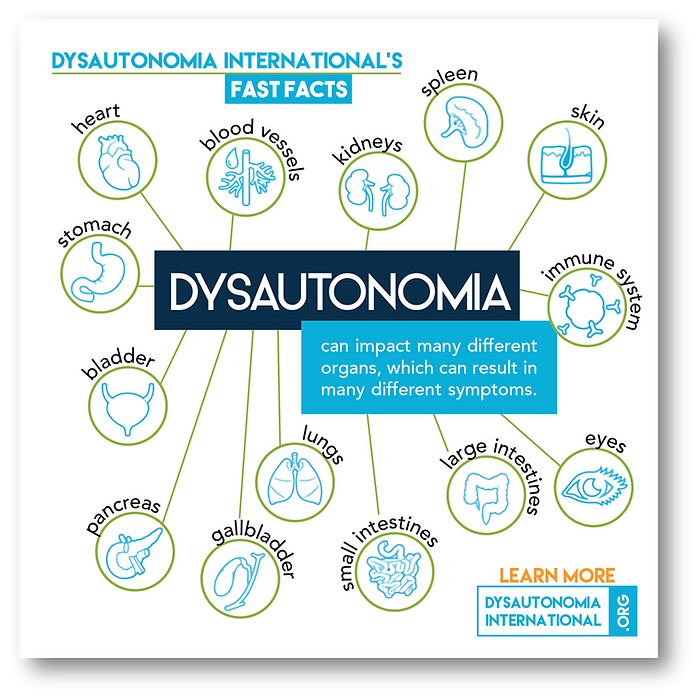
Dysautonomia refers to a group of conditions where the autonomic nervous system malfunctions, affecting processes like heart rate, blood pressure, and digestion. According to Dysautonomia International, the ANS is responsible for bodily functions that happen automatically, such as breathing, temperature regulation, and the heart beating. When dysautonomia develops, these essential functions go haywire, leading to a cascade of symptoms that affect multiple organs and systems in the body.
Since the symptoms can manifest in different ways, it is often difficult to diagnose dysautonomia. This article aims to shed light on the condition, making it easier to identify and understand the key indicators..

Common Dysautonomia Symptoms
Dysautonomia symptoms can vary greatly depending on the severity of the condition and which systems are affected. Here are some of the most common symptoms that people experience:
1. Rapid Heart Rate (Tachycardia):
A quickened heart rate, especially when standing up, is a classic symptom of dysautonomia. This can be a result of the body’s failure to regulate heart rate in response to changes in posture, known as postural orthostatic tachycardia syndrome (POTS).
2. Orthostatic Hypertension:
Many individuals with dysautonomia experience sudden spikes in blood pressure when they stand up. This can lead to dizziness, headaches, and even fainting spells.
3. Chronic Fatigue:
Severe fatigue is common, as the body works overtime trying to regulate autonomic functions. Dysautonomia can feel like an invisible force constantly draining your energy, making it hard to complete everyday tasks.
4. Anxiety and Panic Attacks:
Because dysautonomia affects the nervous system, it can mimic the symptoms of anxiety or panic attacks. Many patients are misdiagnosed with psychological issues before they realize the root cause lies in the ANS.
5. Temperature Dysregulation:
Some individuals struggle with maintaining a consistent body temperature. Cold hands and feet, or overheating, are common dysautonomia symptoms.
6. Shortness of Breath (Dyspnea):
Difficulty breathing or feeling winded even without exertion is often reported by people with dysautonomia. This may be linked to poor regulation of the respiratory system.
7. Gastrointestinal Issues:
Irritable bowel syndrome, bloating, nausea, and other digestive disorders can be signs of autonomic dysfunction. The gut is highly innervated by the nervous system, and when it misfires, gastrointestinal problems often arise.
8. Migraines and Dizziness:
Frequent migraines or feeling light-headed are both common dysautonomia symptoms. These can be triggered by poor blood flow regulation to the brain.
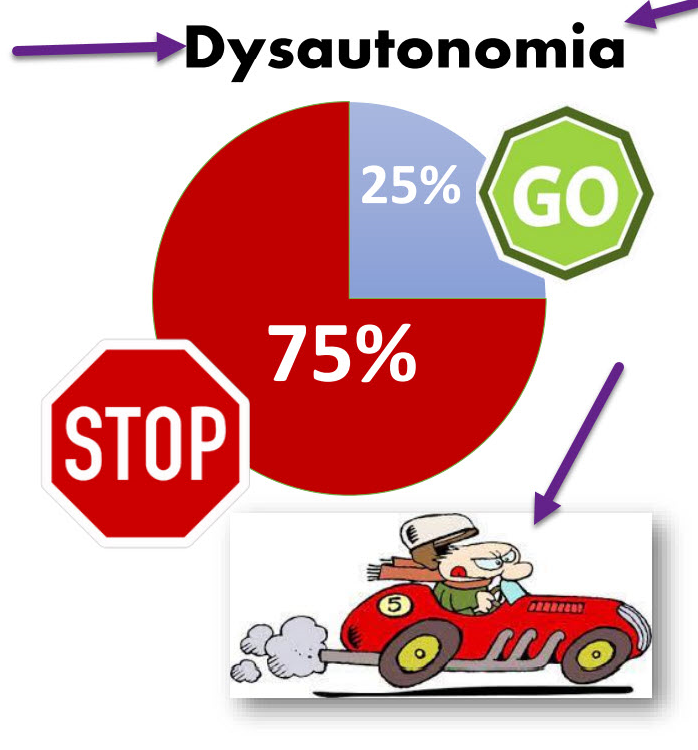
THIS IS WHAT YOU WANT SLOW!

You DON’T want FAST
Causes of Dysautonomia
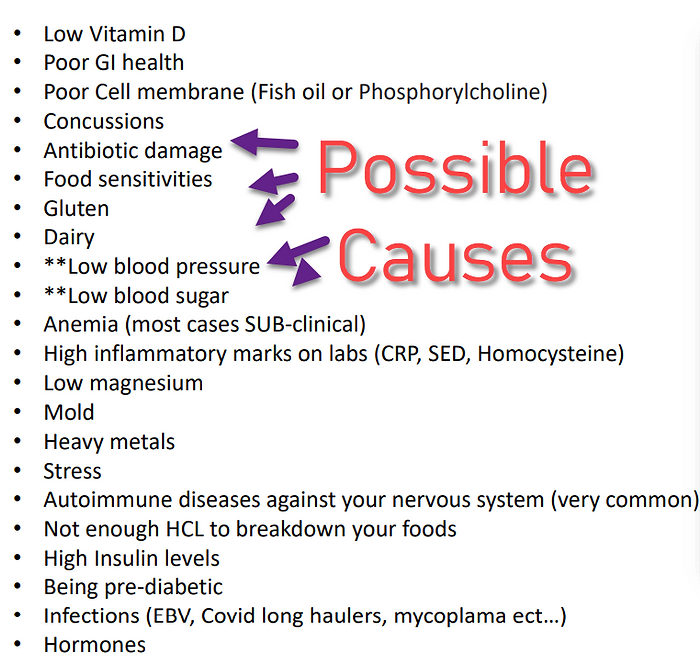
From my experience, I’ve found that 100% of my clients with dysautonomia have at least one contributing factor affecting their nervous system. These causes range from minor issues to more severe health problems. Some common triggers for dysautonomia include:
- Nutritional Deficiencies: Low levels of Vitamin D, magnesium, or other essential nutrients can lead to nervous system issues.
- Gastrointestinal Problems: Poor gut health can disrupt autonomic functions. Inflammation from food sensitivities or infections plays a significant role.
- Concussions or Traumatic Brain Injuries: Damage to the brain can cause long-term autonomic dysfunction.
- Fluoroquinolone Toxicity: Exposure to certain antibiotics like fluoroquinolones has been linked to dysautonomia.
- Chronic Infections: Infections such as Epstein-Barr virus (EBV) or long-haul COVID can disrupt the nervous system.
- Autoimmune Disorders: Your body may develop antibodies that attack the nervous system, leading to dysautonomia.
- Stress and Mental Health Issues: Chronic stress has a direct impact on the autonomic nervous system. Mental health disorders may also play a role in dysautonomia onset.
Fluoroquinolone Toxicity and Dysautonomia
Fluoroquinolones, a class of antibiotics, have been linked to causing dysautonomia in some patients. These antibiotics, while effective in treating bacterial infections, can have severe side effects, including damage to the nervous system. Known as being “floxed,” those affected by fluoroquinolone toxicity may experience long-term effects on their autonomic functions, leading to symptoms such as chronic pain, fatigue, and nerve damage.
Treatment for Fluoroquinolone Toxicity
If you have been affected by fluoroquinolone toxicity, it’s essential to work on detoxifying the body and supporting nerve healing. Treatments may include:
- Magnesium Supplements: Fluoroquinolones deplete magnesium levels, so restoring this mineral can help alleviate symptoms.
- Antioxidant Therapy: Vitamins C and E are crucial for combating oxidative stress caused by antibiotic toxicity.
- Physical Therapy: To help restore nerve function and build strength, working with a physical therapist may aid recovery.
- Dietary Changes: Eliminate inflammatory foods such as gluten and processed sugars to reduce the load on the body and promote healing.
Dysautonomia, the Midbrain, and the Cerebellum
The central portion of the brain, aptly called the midbrain, is what controls these automatic regulations. If it is not functioning properly, you will likely be experiencing neurological issues that you (and likely your doctors) do not understand.
Similar to the midbrain, the cerebellum is directly connected to your body through the spinal cord. The cerebellum alone has more neurons than the rest of your entire brain combined and acts as a sort of “gatekeeper” between the brain and the body. It regulates the signals and information being passed both ways.
The cerebellum is directly connected to the rest of the body through the spinal cord and nerves. If there is something wrong with the cerebellum, it will have immediate effects on the rest of the body.
This takes the form of problems caused within your parasympathetic and sympathetic nerve systems. The former controls functions related to relaxation and digestion, while the latter is related to your “fight or flight” responses. Dysautonomia often causes problems by activating your sympathetic systems.
What Causes Dysautonomia?
I can confidently say that 100% of clients I work with have some level of dysautonomia. The causes can be minor or major, including:
– Low Vitamin D levels
– Poor GI health
– Poor cell membrane function
– Concussions
– Antibiotic damage
– Food sensitivities (including dairy and gluten)
– Low blood pressure
– Anemia
– High inflammatory marks on labs
– Mold infection
– Heavy metals present in the body
– Stress
– Autoimmune diseases against your own nervous system
– Not enough stomach acid to properly digest food
– High insulin levels
– Being pre-diabetic
– Major infections (EBV, long-haul covid, etc)
Examples of Dysautonomia
While there are many ways these causes may present themselves, here is a simple example of how dysautonomia might be affecting your body.
Let’s say your stomach is not using enough acid to break down food. This keeps the food in your system longer, which allows it to ferment. This fermentation brings with it higher bacteria growth than is necessary. That higher level of bacteria results in more protein being passed into the blood, which can create major inflammation problems throughout the entire body.
Your nervous system is an “all or nothing” system. That means it either is firing completely, or not at all. Dysautonomia lowers your threshold for your nerves to fire, meaning that less stimuli is needed for your brain to act. An example of this might be light or noise sensitivity.
Things to get checked out
What Can You Do?
The first thing to do is get tested and look for the root causes listed above. Finding out what problems are going on in your body will give you a clear idea of how to approach your treatment.
Finding out you suffer from chronic low blood pressure, or subclinical anemia will help you treat your individual problems and allow your body to function properly.
Not all situations require testing. For example, if you consistently suffer from bloating, diarrhea, or other digestive problems then you can likely ascribe your dysautonomia to a GI issue without testing.
You can look for resources on my website or schedule a call with me, and we can discuss what issues you are experiencing. Together we can come up with a treatment plan that can help you on the way to health.
Time Stamps to Find Information Quickly!
[00:00:02] going to be on dysautonomia
[00:01:00] if you have any symptoms that are weird or unusual, you probably have it
[00:01:18] 70 million people suffer from this worldwide
[00:01:45] heart rate, your blood pressure, digestion, dilation of your arteries, constriction of your arteries, your eyes, your kidneys, temperature control
[00:02:30] dysautonomia can impact many different organs
[00:03:15] dysautonomia It’s a problem of the brain
[00:03:30] My heart is racing or I have anxiety
[00:03:45] Functional neurology
[00:04:00] your brain not functioning properly
[00:04:08] People are going to tell you you’re crazy
[00:04:45] This has to do with all your automatic nervous system
[00:05:15] is not functioning properly, you are going to have weird, unexplainable neurological, neurological conditions that no one understands.
[00:05:23] You’re going to go to a neurologist and neurologist
[00:06:45] your cerebellum has more neurons in here than your whole entire brain
[00:07:15] hypotension, chronic fatigue, anxiety, temperature, regulation, shortness of breath, irritable bowel gas, bloating, diarrhea, dizziness and migraines
[00:07:45] And this is relax and digest
[00:07:52] Parasympathetic is relax and digest.
[00:08:45] go, go, go. fight or you’re going to flight
[00:09:00] this part of your nervous system is dysregulated
[00:09:15] constricts your pupils
[00:09:30] stimulates your stomach activity, sympathetic nervous system,
[00:10:15] you wake up with sweats, you get in a crowded place and you get anxiety [00:10:30] more epinephrine and norepinephrine
[00:11:00] fast part of your nervous system is over firing
[00:11:15] root cause of the problem
[00:11:30] Do you have low vitamin D, concussions
[00:11:45] anemia
[00:12:07] Did you take antibiotics, fluoroquinolone toxicity drugs
[00:12:15] low blood pressure
[00:13:30] inflammatory markers , Do you have low magnesium
[00:13:45] Do you have an autoimmune disease against your brain tissue
[00:14:15] sympathetic storm
[00:14:21] not producing enough hydrochloric acid to break down foods
[00:14:45] Are you pre-diabetic
[00:15:30]sympathetic nervous system being increased
[00:15:33] It’s the fast racing car
[00:17:04] This is healthy. And then here we have unhealthy nerves
[00:18:15] unhealthy neuron,
[00:19:15] light sensitive
[00:19:30] brain trauma
[00:21:00] blood pressure right here
[00:21:30] start making ATP and your mitochondria
[00:21:49] too low. Blood pressure should be 120 over 80
[00:22:00] blood up into your brain, hypoglycemia
[00:22:15] anemia
[00:22:30] immune system
[00:22:45] strong or weak immune system
[00:23:00] the nerves going to the heart
[00:23:15] firing that goes your heart, have a racing heart
[00:23:30] You’re going to have sound sensitivity
[00:24:15] 90% of your brain. Is stopping
[00:25:57] most of your brain is stopping things
[00:26:15] You get weird neurological symptoms that no one can explain
[00:29:00] knocked unconscious
[00:29:15] car accident
[00:29:30] balance problems. He has anxiety
[00:30:00] concussions and then you got to clean up your diet
Research Citations
- All that shakes is not epilepsy. Hart YM. J R Coll Physicians Edinb. 2012 Jun; 42(2):151-4.
- Amnesia for loss of consciousness is common in vasovagal syncope. O’Dwyer C, et al. Europace. 2011 Jul; 13(7):1040-5.
- Aortic elastic properties of patients with neurocardiogenic syncope. Sucu MM, et al. Pacing Clin Electrophysiol. 2009 Nov; 32(11):1417-21.
- Are treatments for vasovagal syncope effective? A meta-analysis. Vyas A, et al. Int J Cardiol. 2012 May. [Epub ahead of print]
- Arterial baroreflex function in older adults with neurocardiogenic syncope. Madden KM, Lockhart C. Clin Invest Med. 2009 Jun; 32(3):E191-8.
- Basic autonomic nervous function in patients with neurocardiogenic syncope. Saito F, et al. Clin Exp Hypertens. 2007 Apr; 29(3):165-73.
- Cardiac autonomic disturbances in patients with vasovagal syndrome: comparison between iodine-123-metaiodobenzylguanidine myocardial scintigraphy and heart rate variability. Kochiadakis G, et al. Europace. 2012 Mar. [Epub ahead of print]
- Cardioinhibitory carotid sinus hypersensitivity predicts an asystolic mechanism of spontaneous neurally mediated syncope. Maggi R, et al. Europace. 2007 Aug; 9(8):563-7.
- Catheter ablation of severe neurally meditated reflex (neurocardiogenic or vasovagal) syncope: cardioneuroablation long-term results. Pachon JC, et al. Europace. 2011 Sep; 13(9):1231-42.
- Cerebral blood flow abnormalities in patients with neurally mediated syncope. Joo EY, et al. J Neurol. 2011 Mar; 258(3):366-72.
- Clinical efficacy of beta1 selective adrenergic blockers in the treatment of neurocardiogenic syncope – a meta-analysis. Vallurupalli S, Das S. Clin Pharmacol. 2010; 2:163-7.
- Comparison of recurrence rate based on the frequency of preceding symptoms in patients with neurocardiogenic syncope or presyncope. Lee SM, et al. Korean Circ J. 2011 Aug; 41(8):434-9.
- Dysautonomia: Perioperative Implications. Anesthesiology. 2012 Feb;116;1:205?215
- Endogenous circadian rhythm in vasovagal response to head-up tilt. Hu K, et al. Circulation. 2011 Mar; 123(9):961-70.
- Enhanced vascular responses to hypocapnia in neurally mediated syncope. Norcliffe-Kaufmann LJ, et al. Ann Neurol. 2008 Mar; 63(3):288-94.
- Evaluation of syncope. Gauer RL. Am Fam Physician. 2011 Sep; 84(6):640-50.
- Genetic variation in gsα protein as a new indicator in screening test for vasovagal syncope. Lelonek M, et al. Circ J. 2011; 75(9):2182-6.
- Increased hydration alone does not improve orthostatic tolerance in patients with neurocardiogenic syncope. Bellard E, et al. Clin Auton Res. 2007 Apr; 17(2):99-105.
- Neurally-mediated sincope. Can I, et al. Minerva Med. 2009 Aug; 100(4):275-92.
- Neurocardiogenic syncope coexisting with postural orthostatic tachycardia syndrome in patients suffering from orthostatic intolerance: a combined form of autonomic dysfunction. Kanjwal K, et al. Pacing Clin Electrophysiol. 2011 May; 34(5):549-54.
- Pharmacotherapy of autonomic failure. Shibao C, et al. Pharmacol Ther. 2012 Jun; 134(3):279-86.
- Physiological phenomenology of neurally-mediated syncope with management implications. Schroeder C, et al. PLoS One. 2011; 6(10):e26489.
- Positive result in the early passive phase of the tilt-table test: a predictor of neurocardiogenic syncope in young men. Uhm JS, et al. Korean J Intern Med. 2012 Mar; 27(1):60-5.
- Recognition and management of complications during moderate and deep sedation. Part 2: cardiovascular considerations. Becker DE, et al. Anesth Prog. 2011 Fall; 58(3):126-38.
- Respiration drives phase synchronization between blood pressure and RR interval following loss of cardiovagal baroreflex during vasovagal syncope. Ocon AJ, et al. Am J Physiol Heart Circ Physiol. 2011 Feb; 300(2):H527-40.
- Symptoms and signs of syncope: a review of the link between physiology and clinical clues. Wieling W, et al. Brain. 2009 Oct; 132(Pt 10):2630-42.
- Syncopal migraine. Curfman D, et al. Clin Auton Res. 2012 Feb; 22(1):17-23.
- The changing face of orthostatic and neurocardiogenic syncope with age. Cooke J, et al. QJM. 2011 Aug; 104(8):689-95.
- The effect of paediatric syncope on health-related quality of life. Anderson JB, et al. Cardiol Young. 2012 Feb. [Epub ahead of print]
- The influence of vasovagal response on the coagulation system. Kraemer M, et al. Clin Auton Res. 2010 Apr; 20(2):105-11.
- The origin of vasovagal syncope: to protect the heart or to escape predation? Alboni P, et al. Clin Auton Res. 2008 Aug; 18(4):170-8.
- Therapy of vasovagal syncope: to prevent the vasovagal reflex or to treat the impending reflex? Alboni P. Europace. 2010 Jun; 12(6):776-8.
- Vasovagal syncope and vasovagal disease. Brignole M. Hellenic J Cardiol. 2008 Mar; 49(2):61-4.
- Vulnerability to simple faints is predicted by regional differences in brain anatomy. Beacher FD, et al. Neuroimage. 2009 Sep; 47(3):937-45.
- What Happens before Syncope? Study of the Time Frame Preceding Vasovagal Syncope. Lagi A, et al. ISRN Cardiol. 2011; 2011:659787.